The University of Wisconsin-Madison has conducted a study showing that wearing facemasks in the classroom setting can be highly effective at reducing the aerosol transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).

However, the filtration efficiency of facemasks can below if they are not fitted properly, warns David Rothamer and colleagues.
The researchers also demonstrated that classroom ventilation alone did not sufficiently reduce the infection probability, whereas even the use of only moderately effective facemasks did reduce this probability sufficiently.
A pre-print version of the paper is available on the medRxiv* server while the article undergoes peer review.
Using the Wells-Riley equation to assess aerosol transmission
Since the first cases of SARS-CoV-2 were identified in Wuhan, China late last year (2020), researchers have increasingly recognized the long-range airborne route of viral transmission and the need for effective measures to block this transmission mode.
A common approach for assessing long-range airborne transmission (referred to hereafter as aerosol transmission), uses the Wells-Riley equation to relate aerosol concentrations to infection probability.
This approach has already been widely applied in studies of SARS-CoV-2, particularly in the context of super-spreader events.
The researchers say the application of the Wells-Riley equation is useful for risk assessment and the planning of interventions to reduce the risk of disease transmission.
What did the researchers do?
The team applied the Wells-Riley equation to evaluate the effect of ventilation, mask filtration, and a combination of the two on aerosol SARS-CoV-2 infection probability in the classroom setting.
A polydisperse neutralized salt (NaCl) aerosol that was generated in a size range consistent with SARS-CoV-2-containing bioaerosols was used as a safe surrogate for measurements.
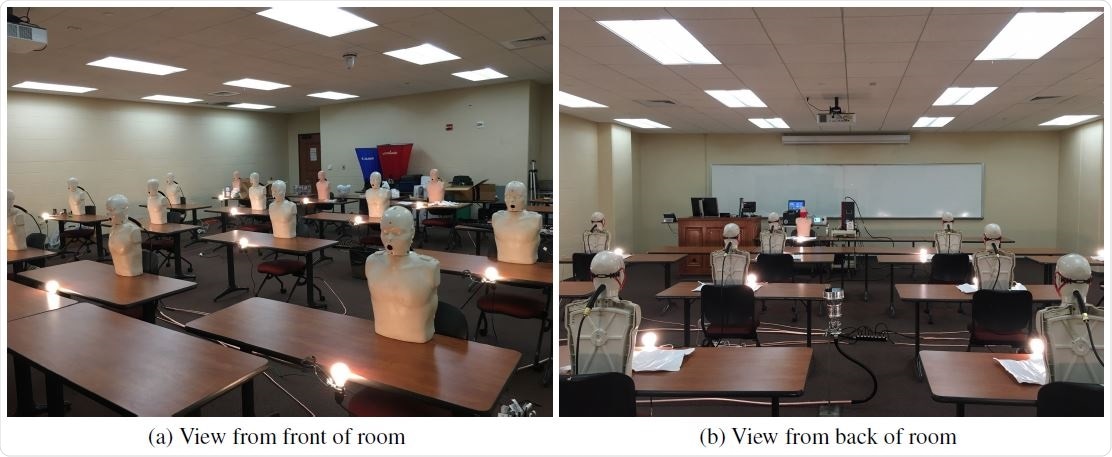
The mask effective filtration efficiency was tested by seeding a classroom with the NaCl aerosol and sampling concentrations of the aerosol through four different mask types that had been fitted to manikins with and without using mask fitters.
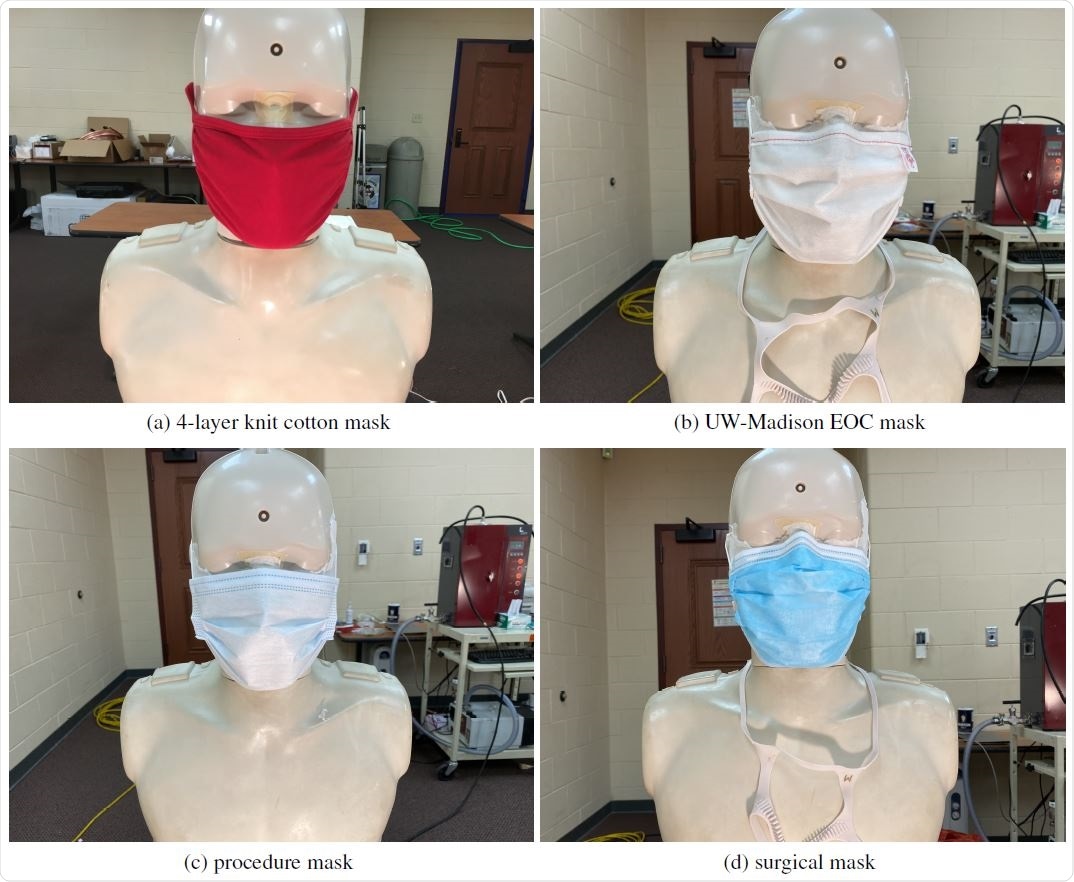
Two of the masks were washable reusable masks. One was made of 4-layers of knit cotton, and the other was made of 3-layers of non-woven spun-bond polypropylene.
The other two masks were disposable. One was a common single-use disposable mask (referred to hereafter as procedure mask), and the other was an ASTM F2100 level-2 surgical mask.
The importance of masks fitting properly
Measurements of the mask's effective filtration efficiency demonstrated the importance of masks being fitted properly. Poorly fitting masks exhibited filtration efficiencies that decreased by as much as a factor of six. The estimated leakage rate for most of the poorly fitted masks was typically more than 50%.
The analysis also found that the knit-cotton mask was only able to achieve an effective filtration efficiency of 26%, even when a mask fitter was used.
In all other cases, the use of a mask fitter significantly improved the effective filtration efficiency, with the exception of the polypropylene mask, which achieved a good fit without a mask fitter. In the case of the procedure mask, the use of a mask fitter achieved effective filtration efficiencies of almost 95%.
Classroom ventilation alone was insufficient
The study also suggested that classroom ventilation alone was not sufficient to achieve infection probabilities of less than 1%.
On the other hand, the use of moderate-to-high effective filtration efficiency masks by all individuals (manikins) present significantly reduced the infection probability.
Depending on the type of mask and whether a mask fitter was used, infection probability was reduced by 5-, 10- or even more than 100-fold.
The team says infection probabilities of less than 0.1% and even lower than 0.0001% could be reached with the use of masks and mask fitters alone.
What does the team advise?
Rothamer and colleagues say the results reinforce the use of properly donned masks to achieve reduced aerosol transmission of SARS-CoV-2.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Rothamer D, et al. Strategies to minimize SARS-CoV-2 transmission in classroom settings: Combined impacts of ventilation and mask effective filtration efficiency. medRxiv, 2020. https://www.medrxiv.org/content/10.1101/2020.12.31.20249101v1










