(CNN)India is embarking on one of the world's most ambitious mass immunization programs ever undertaken after regulators approved the country's first two Covid-19 vaccines for restricted emergency use.
January 08, 2021
India embarks on one of the world's most ambitious vaccine rollouts after emergency use approval
January 08, 2021The University of Wisconsin-Madison has conducted a study showing that wearing facemasks in the classroom setting can be highly effective at reducing the aerosol transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).

However, the filtration efficiency of facemasks can below if they are not fitted properly, warns David Rothamer and colleagues.
The researchers also demonstrated that classroom ventilation alone did not sufficiently reduce the infection probability, whereas even the use of only moderately effective facemasks did reduce this probability sufficiently.
"The results reinforce the use of properly donned masks to achieve reduced aerosol transmission of SARS-CoV-2 and other infectious diseases transmitted via respiratory aerosol indoors," writes the team.
A pre-print version of the paper is available on the medRxiv* server while the article undergoes peer review.
Using the Wells-Riley equation to assess aerosol transmission
Since the first cases of SARS-CoV-2 were identified in Wuhan, China late last year (2020), researchers have increasingly recognized the long-range airborne route of viral transmission and the need for effective measures to block this transmission mode.
A common approach for assessing long-range airborne transmission (referred to hereafter as aerosol transmission), uses the Wells-Riley equation to relate aerosol concentrations to infection probability.
This approach has already been widely applied in studies of SARS-CoV-2, particularly in the context of super-spreader events.
The researchers say the application of the Wells-Riley equation is useful for risk assessment and the planning of interventions to reduce the risk of disease transmission.
"One of the aims of this paper is to provide recommendations that, when implemented, can decrease the likelihood of COVID-19 transmission in traditionally high occupancy spaces such as classrooms," they write.
What did the researchers do?
The team applied the Wells-Riley equation to evaluate the effect of ventilation, mask filtration, and a combination of the two on aerosol SARS-CoV-2 infection probability in the classroom setting.
Related Stories
A polydisperse neutralized salt (NaCl) aerosol that was generated in a size range consistent with SARS-CoV-2-containing bioaerosols was used as a safe surrogate for measurements.
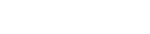
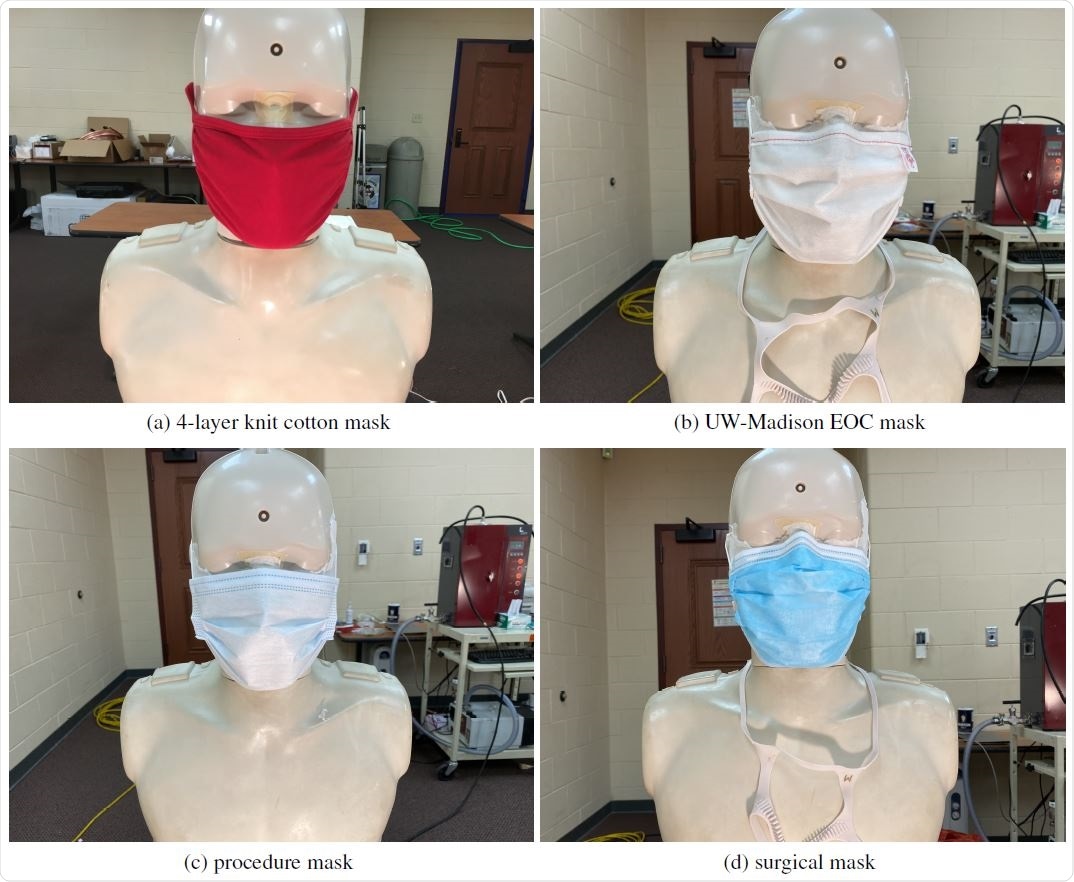
The mask effective filtration efficiency was tested by seeding a classroom with the NaCl aerosol and sampling concentrations of the aerosol through four different mask types that had been fitted to manikins with and without using mask fitters.
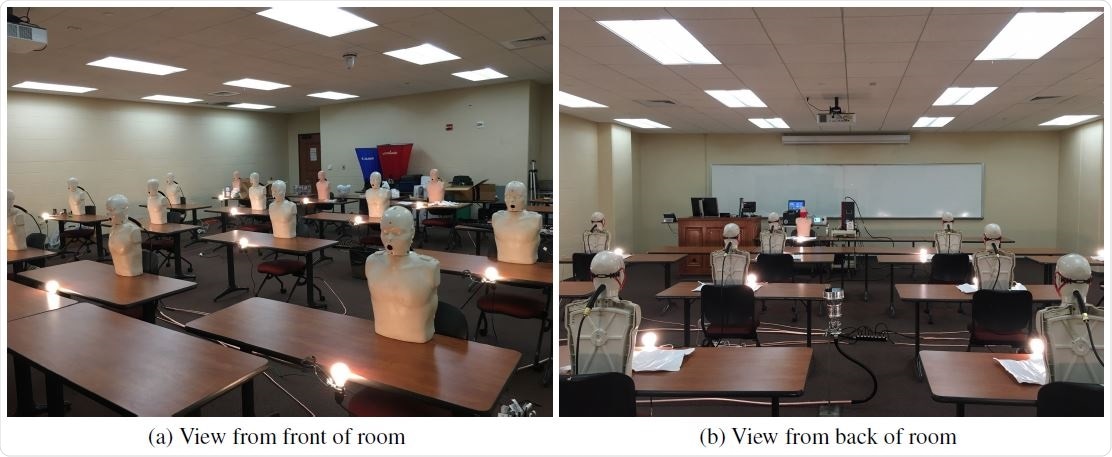
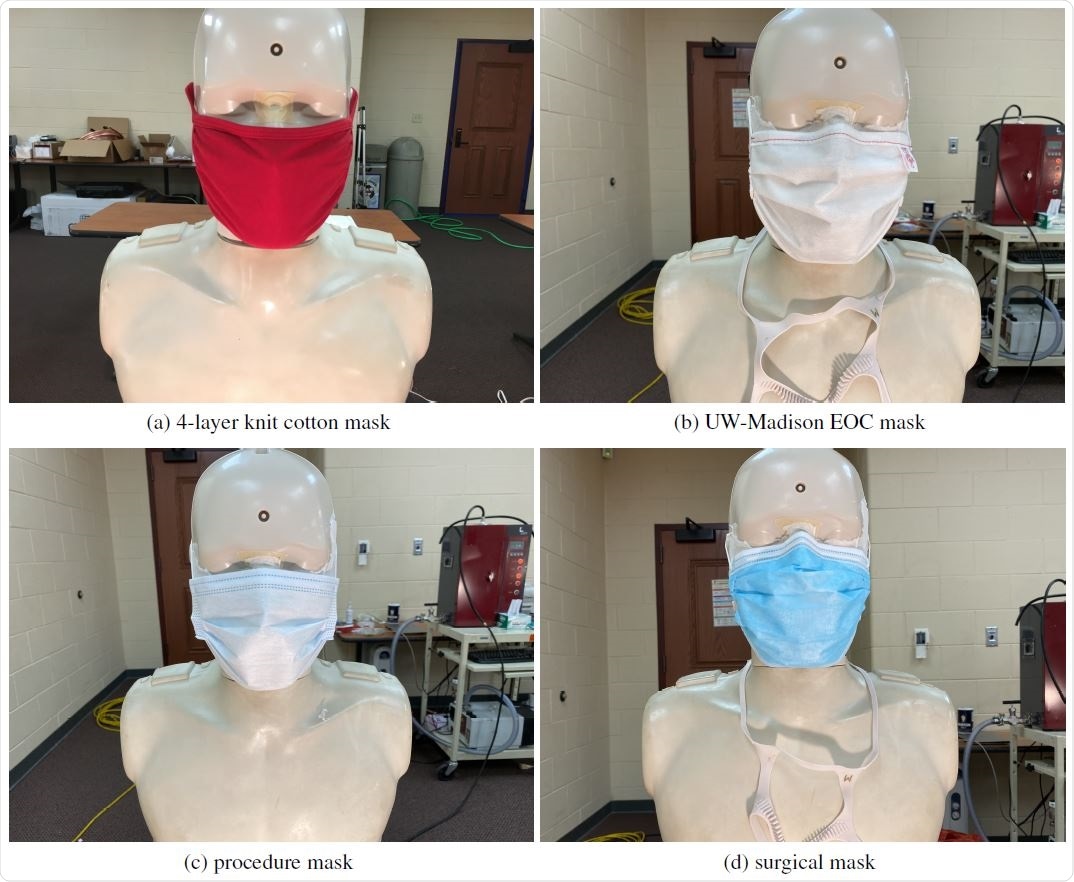
Two of the masks were washable reusable masks. One was made of 4-layers of knit cotton, and the other was made of 3-layers of non-woven spun-bond polypropylene.
The other two masks were disposable. One was a common single-use disposable mask (referred to hereafter as procedure mask), and the other was an ASTM F2100 level-2 surgical mask.
The importance of masks fitting properly
Measurements of the mask's effective filtration efficiency demonstrated the importance of masks being fitted properly. Poorly fitting masks exhibited filtration efficiencies that decreased by as much as a factor of six. The estimated leakage rate for most of the poorly fitted masks was typically more than 50%.
The analysis also found that the knit-cotton mask was only able to achieve an effective filtration efficiency of 26%, even when a mask fitter was used.
In all other cases, the use of a mask fitter significantly improved the effective filtration efficiency, with the exception of the polypropylene mask, which achieved a good fit without a mask fitter. In the case of the procedure mask, the use of a mask fitter achieved effective filtration efficiencies of almost 95%.
Classroom ventilation alone was insufficient
The study also suggested that classroom ventilation alone was not sufficient to achieve infection probabilities of less than 1%.
On the other hand, the use of moderate-to-high effective filtration efficiency masks by all individuals (manikins) present significantly reduced the infection probability.
Depending on the type of mask and whether a mask fitter was used, infection probability was reduced by 5-, 10- or even more than 100-fold.
The team says infection probabilities of less than 0.1% and even lower than 0.0001% could be reached with the use of masks and mask fitters alone.
What does the team advise?
Rothamer and colleagues say the results reinforce the use of properly donned masks to achieve reduced aerosol transmission of SARS-CoV-2.
"The results specifically emphasize the large potential for effective mask-wearing and improved masks, or use of mask fitters, to greatly reduce infection probabilities," concludes the team.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Rothamer D, et al. Strategies to minimize SARS-CoV-2 transmission in classroom settings: Combined impacts of ventilation and mask effective filtration efficiency. medRxiv, 2020. https://www.medrxiv.org/content/10.1101/2020.12.31.20249101v1
January 15, 2017
What Causes Obesity?
"What causes a person to become obese?"
Obesity occurs when, over a long period of time, the amount of food we put into our bodies each day is not used. In essence, this means that there consistently is more energy going in, than out. That energy has to go somewhere, so our bodies store it as fat.
Energy In vs Energy Out Equation
ENERGY "IN" MORE THAN ENERGY "OUT" = WEIGHT GAIN.
ENERGY "IN" LESS THAN ENERGY "OUT" =WEIGHT LOSS.
We all overindulge every now and then, and it isn’t this occasional overeating that causes obesity; obesity is caused when we overdo it most days, for a sustained period of time.
Unfortunately, we live in an environment that encourages us to eat and discourages us to be active, making it very easy to gain weight.
Have a think about it…
Food is readily available, 24 hours a day, 7 days a week Portion sizes and plates are much bigger than they have been before we can get almost anywhere without having to walk or use a bikeTVs, computers and mobile phones encourage a more sedentary lifestyle.
October 04, 2010
Daniel Mackay, PhD, from the University of Glasgow, in Scotland, and colleagues reported the findings in the September 16 issue of the New England Journal of Medicine.
According to the researchers, the Smoking, Health and Social Care (Scotland) Act banned smoking in all enclosed public places and workplaces in Scotland as of March 26, 2006.
"The legislation has been extremely successful in its primary aim of reducing exposure to environmental tobacco smoke in public places, such as bars," the authors note. In addition, the legislation has reduced exposure of children to environmental tobacco smoke, despite concerns of smoking being displaced to the home, but it is unclear whether the risk for childhood asthma has also decreased.
The researchers collected routine hospital administrative data and ascertained all hospital admissions for asthma in Scotland from January 2000 through October 2009 among children younger than 15 years.
Before the smoking ban, asthma admissions were increasing by an average of 5.2% per year (95% confidence interval [CI], 3.9% - 6.6%). After the ban, the rate of admissions decreased by 18.2% per year relative to the rate on March 26, 2006 (95% CI, 14.7% to 21.8%; P < .001). Rates were reduced both in preschool and school-age children.
Various factors including age group, sex, urban or rural residence, region, or quintile of socioeconomic status had no effect on the outcome.
Limitations of the study include that only exacerbations severe enough to warrant hospitalization were included. In addition, information regarding individual smoking status was not available; therefore, whether the observed reduction in asthma was a result of reduced exposure to environmental tobacco smoke in the home, reduced exposure to environmental tobacco smoke in public places, a reduction in active smoking among school-age children, or an unrelated cause cannot be determined.
"After the introduction of comprehensive smoke-free legislation, there was a reduction in the incidence of asthma among people who did not have occupational exposure to environmental tobacco smoke," the authors conclude.
They add that the "overall exposure of children to environmental tobacco smoke, measured objectively with the use of salivary cotinine concentrations, has fallen since the implementation of the Scottish legislation."
The study was supported by a project grant from National Health Services Health Scotland. One author reports individual employment by National Health Services Scotland; another chairs the Committee on Medical Effects of Air Pollution for the UK Department of Health. The other authors have disclosed no relevant financial relationships.
N Engl J Med. 2010;363:1139-1145.
September 26, 2010
"[MSM] are at increased risk for infection with [HIV]," write A. Smith, MPH, and colleagues from the Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, US Centers for Disease Control and Prevention (CDC). "In 2006, 57% of new HIV infections in the United States occurred among MSM."
The CDC uses the National HIV Surveillance system (NHBS) to monitor prevalence and trends in HIV-related risk behaviors, HIV testing, and use of HIV prevention services among high-risk populations. In the current report, the authors summarize NHBS data from 2008.
From January to December 2008, 8153 MSM from 21 cities were interviewed and tested for HIV. The study found that the overall prevalence of HIV was 19%.
Non-Hispanic blacks had the highest prevalence (28%), followed by Hispanics (18%), non-Hispanic whites (16%), and persons who were multiracial or of other race (17%).
Forty-four percent of those infected with HIV were unaware of their status. Black MSM with HIV were least likely to be aware of their infection (59%), followed by Hispanic MSM (46%) and white MSM (26%).
The study also found that although young men, aged 30 years or younger, had a lower HIV prevalence than older men, they were much more likely to be unaware of their HIV infection. Among men aged 18 to 29 years who had HIV, 63% were unaware vs 37% of men aged 30 years and older.
Also among young men, MSM of color were less likely than their white counterparts to know they were infected with HIV. Among blacks aged 30 years or younger, 71% were unaware of their status compared with 63% of young Hispanic MSM and 40% of young white MSM.
The study also found a strong link between socioeconomic status and HIV infection in MSM. The prevalence of HIV infection increased as education and income decreased, as did awareness. These findings are similar to those found in recent NHBS research among homosexuals, the authors report.
Men who know their current HIV infection status can be referred to appropriate medical care and prevention services. Once they are linked to prevention services, they can learn ways to avoid transmitting HIV to others, the authors note, adding that efforts to reach out to young and minority MSM should be increased to promote testing for HIV.
The authors also note limitations of their report. Because interviewers conducted the surveys, positive HIV status might have been underreported. Also, because the findings are limited to men who frequented bars, dance clubs, and other MSM venues, they may not be representative of results for all MSM.
"The high proportion of MSM unaware of their HIV infection continues to be a serious public health concern, because these MSM account for the majority of estimated new HIV transmissions in the United States," the author write in their concluding remarks. "The 2008 NHBS data show that MSM remain a key target of strategies to reduce HIV incidence and decrease racial and socioeconomic disparities in the United States."
"This study's message is clear: HIV exacts a devastating toll on [MSM] in America's major cities, and yet far too many of those who are infected don't know it," Kevin Fenton, MD, director of the CDC's National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said in a statement. "We need to increase access to HIV testing so that more MSM know their status, and we all must bring new energy, new approaches, and new champions to the fight against HIV among [MSM]."
The authors have disclosed no relevant financial relationships.
Morb Mortal Wkly Rep. 2010;59:1201-1207
September 22, 2010
Compared with patients without depression and CHD, the risk for all-cause mortality was 3 times higher, and the risk for cardiovascular disease mortality 4 times higher, in patients who had both, after adjusting for age and sex, report Hermann Nabi, MD, from Hôpital Paul-Brousse, Villejuif, Paris, France, and colleagues.
"This study provides further evidence that the relationship between depression and morbidity–mortality is real," Dr. Nabi told Medscape Medical News.
Depression and mortality have been studied separately in patients with CHD and in healthy patients, but this does not allow comparisons across risk-factor groups according to depression and CHD status.
In the study, Dr. Nabi and his team examined the effects of both on mortality in 5936 middle-aged men and women whose mental and physical health were followed-up for a mean of 5.6 years.
The study population was part of the Whitehall II cohort study, a longitudinal study established in 1985 to examine the effect of social and economic factors on the long-term health of 10,308 civil servants who were aged between 35 and 55 years at the start of the study.
Of the 5936 individuals, 170 died during follow-up; 47 of those deaths were from cardiovascular disease.
The analysis showed that the prevalence of depression was 14.9%, and participants with a history of CHD were more likely to have depressive symptoms (20% vs 14%; P = .001) than those without CHD.
The age- and sex-adjusted hazard ratios for all-cause mortality were 1.67 (P < .05) for participants with CHD only, 2.10 (P < .001) for those with depressive symptoms only, and 4.99 (P < .001) for those with both CHD and depressive symptoms compared with participants who were free of both conditions.
Need for a More Integrated Approach
The study findings have implications for research and clinical practice, Dr. Nabi said.
"For research, this study shows that the mechanisms underlying the association between depression and adverse health outcomes such as mortality are still in need of comprehensive studies."
For clinical practice, it implies the need for a more integrated approach in the healthcare system and a shift toward a more "mind–body medicine' approach.
An important step would be to identify cardiac patients who also have depression, he said.
"In this study, the depression worsened heart disease, because we observed that participants with both depression and heart disease were at increased risk for death when compared with those with heart disease only. So we should identify those cardiac patients who have clinically significant depressive symptoms."
Dr. Nabi expressed the wish that his study findings will prompt clinicians to be aware of and look for depression in their patients with heart disease.
"Even though there is no consensus at the moment, healthcare professionals should screen and treat, or refer to treatment. Simple screening tools exist, and [clinicians] should refer their depressed patients, particularly if an adequate referral for systematic depression assessment and treatment is readily available."
He also discussed some limitations of the study.
"This study is based on a cohort of civil servants and did not include blue-collar workers, unemployed, or individuals with precarious jobs. This may have underestimated the magnitude of associations observed in our study because of the prevalence of depression and the mortality rate is higher in these latter individuals. Thus, it is reasonable to assume that the effect of depression would be greater in studies including various populations."
Randomized Trial Required
"This paper is adding to a literature that is imperfect. It makes you feel more confident about the literature," Alexander H. Glassman, MD, chief of clinical psychopharmacology at New York State Psychiatric Institute and professor of psychiatry at Columbia University, New York City, commented to Medscape Medical News.
"There are literally a hundred, maybe more, studies indicating that depression and heart disease are related," Dr. Glassman, who was not part of the current study, noted. "There are a handful of studies that do not find a relationship, but they are vastly outnumbered by the ones that have found a relationship."
However, he pointed out, just because there is an association that does not mean one condition causes the other. The way to prove cause would be with a randomized controlled trial.
"It's very easy to think depression is increasing the risk or is a cause of subsequent heart disease. And let me say, I think it is," said Dr. Glassman, who led the placebo-controlled Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), as reported by Medscape Medical News.
SADHART found that patients hospitalized for acute coronary syndrome who also have major depression are twice as likely to die within 7 years if their depression did not significantly improve.
"The best way to know for sure would be to do a randomized trial on the treatment for depression with a placebo control. If you reduced the depression and those people with an antidepressant effect had a lower mortality, then you would have unequivocal evidence that depression is causing death, because by getting rid of it, you reduce the chance of dying."
The study was funded by the Medical Research Council, British Heart Foundation, Health and Safety Executive, Department of Health, National Heart Lung and Blood Institute, National Institute on Aging, Agency for Health Care Policy Research, and John D. and Catherine T. MacArthur Foundation Research Networks on Successful Midlife Development and Socio-economic Status and Health. Dr. Nabi has disclosed no relevant financial relationships. Dr. Glassman reports financial relationships with Pfizer Inc.
Heart. Published online September 16, 2010.
September 19, 2010
"In clinical trials of drug treatments for women's sexual dysfunction, placebo responses have often been substantial," write Andrea Bradford, PhD, from Baylor College of Medicine in Houston, Texas, and Cindy M. Meston, PhD, from the University of Texas at Austin. "However, little is known about the clinical significance, specificity, predictors, and potential mechanisms of placebo response in sexual dysfunction."
The goal of the study was to evaluate the characteristics and predictors of sexual function outcomes in 50 women with FSAD who were randomly assigned to the placebo group of a 12-week, multisite, controlled pharmaceutical trial. Magnitude, domain specificity, and clinical significance of sexual function scores were evaluated at baseline and at 4, 8, and 12 weeks (after study completion).
Change with time in sexual function outcomes was assessed in relationship to several variables, including age and symptom-related distress at baseline, as well as changes in frequency of sexual behavior during the trial. The primary study endpoint was the total score on the Female Sexual Function Index.
"It's important to note that, even though these women received placebo, they all had an opportunity to talk to a health provider about their difficulties and were asked to closely monitor their sexual behavior and feelings over a 12-week period," Dr. Bradford said in a news release. "Just taking part in this study probably started some meaningful conversations."
Approximately one third of women receiving placebo had a clinically significant magnitude of change after study completion, with similar effect sizes across multiple aspects of sexual function. Although symptom improvement was strongly associated with the frequency of satisfying sexual encounters (SSEs) during treatment, there was significant variation between participants in the association between frequency of sexual encounters and outcome.
"Our study shows that even a limited intervention can have a positive effect in many women with sexual dysfunction," Dr. Bradford said. "This comes as no surprise to sex therapists, but it does suggest a need to investigate behavioral factors more closely in clinical trials."
Limitations of this study include observational design, precluding determination of causality; and the possibility that SSE frequency was just a proxy for another variable, such as changes in general relationship functioning. In addition, the retrospective analysis prevented direct manipulation of variables of interest, and it is not known whether trial participants who received no treatment would have reported the same effects as participants who received placebo.
"A substantial number of women experienced clinically significant improvement in sexual function during treatment with placebo," the study authors write. "Changes in sexual behavior during the trial, more so than participant age or symptom severity at baseline, appeared to be an important determinant of outcome. Contextual and procedural aspects of the clinical trial may have influenced outcomes in the absence of an active drug treatment."
Eli Lilly/ICOS shared the data set used in this study. This study was supported in part by the Houston VA HSR&D Center of Excellence. The views expressed in the journal article are those of the study authors and do not necessarily represent the views of the Department of Veterans Affairs. Drs. Bradford and Meston have disclosed no relevant financial relationships.
J Sex Med. Published online September 16, 2010.
The data are reported in the September issue of the European Journal of Cancer, which is dedicated to cancer prevention.
An increasing proportion of the European population now has a body mass index (BMI) higher than 25 kg/m2, and few Europeans are engaging in the amounts of physical activity recommended by current guidelines (at least 30 minutes of moderate-intensity activity 5 or more days a week), the researcher note.
The researchers set out to predict what would happen if the European population managed to maintain a mean BMI of 21 kg/m2 and if all countries had a level of physical activity similar to that seen in the Netherlands, where both cycling and walking are popular.
They used the PREVENT statistical modeling method, which was developed at Erasmus University in the Netherlands and is frequently used in the European Union's EUROCADET project.
"We know that large numbers of colon cancer cases could be avoided by reducing exposure to risk factors," said senior author Andrew Renehan, PhD, FRCS, FDS, from the School of Medicine, University of Manchester, United Kingdom. And 2 of the most easily controllable risk factors are physical inactivity and excess weight, he added.
"The predictive modeling is beginning to tease out the independent relevance of each of these factors in the prevention of colon cancer," he said in a statement.
"Preventing weight gain and encouraging weight reduction seem to be most beneficial in men, but for women a strategy with a greater emphasis on increasing physical activity would be more effective," he explained.
Colon Cancer Increasing
Colon cancer rates are increasing in Europe; they have been on the rise since 1975. It is the second most common cancer in Europe and the second most common cause of cancer death, the researchers note.
In a previous study, Dr. Renehan and colleagues attributed the increasing rates of all cancers to increasing obesity in European countries. They estimated that in 2008, new cancers attributed to excess body weight affected 3.2% of women and 8.6% of men; this was an increase from the estimates for 2002, which projected that excess weight was related to new cancers in 2.5% of men and 4.1% of women.
Those data were presented at the 2009 meeting of the European Cancer Organization, and reported by Medscape Medical News at the time.
"People in Europe are gaining weight," Dr. Renehan said at the time, "and it is projected to keep rising."
In the new study, the researchers used the computer model to look at what would happen if Europeans continued to grow fatter, using a hypothetical scenario in which obesity levels increased at the same rate as they have in the United States. They predicted that this would lead to an increase in the number of new colon cancer cases of between 0.7% and 3.8%, depending on the European country.
Then they hypothesized a scenario in which Europeans managed to control their weight and managed to achieve an optimum BMI of 21 kg/m2. They calculated that by the year 2040, this weight-control strategy would prevent between 2% and 18% of colon cancer cases across the countries they studied. The benefits were much higher for males (13.5% to 18%) than for females (2.3% to 4.6%), and most benefit would be seen in British males (in whom 18% of new colon cancer cases could be prevented).
This "underlines the importance of stopping and reversing the ongoing increase in overweight and obesity prevalence," the authors note.
When the team considered physical activity, they found that the Netherlands had the highest rates, which they attributed to a high frequency of bike use, often as a means of transportation. They also found high levels of walking.
Using the Netherlands as the ideal, the researchers predicted what would happen if other countries adopted the same amount of physical activity. They found that overall, 17.5% of new colon cancer cases could be prevented by 2040, with the most benefit in Spanish females (in whom 21% of new colon cancer cases could be prevented).
"We can safely say that increasing physical activity across Europe to the level already achieved in the Netherlands, where everyone cycles, would be of substantial benefit," said coauthor Jan-Willem Coebergh, MD, PhD, from Erasmus University.
"In summary, the changes in physical activity and/or mean levels of overweight in the selected European populations would result in quite substantial effects on future colon cancer rates," the authors conclude.
The researchers have disclosed no relevant financial relationships.
Eur J Cancer. 2010;46:2605-2616.
"Despite recent Centers for Disease Control and Prevention guidelines urging health care personnel with flu-like illness to avoid working, presenteeism (working while sick) is prevalent among health care workers," write Anupam B. Jena, MD, PhD, from Massachusetts General Hospital in Boston, and colleagues. "Ill health care workers can endanger patients and colleagues due to decline in performance or spread of disease. Resident physicians may face unique pressures to work when sick and lack time to seek health care."
The study goal was to evaluate self-reported presenteeism rates and associated factors among residents in a sample of programs selected for varied geographic, size, and governance characteristics. A 50-item survey was administered anonymously in August 2009 to 744 residents in postgraduate year (PGY) 2 and 3 in general surgery, obstetrics/gynecology, internal medicine, and pediatrics at 35 programs in 12 hospitals regarding presenteeism during the prior year. Overall response rate was 72.2% (range among hospitals, 48% - 100%).
More than half of responders (57.9%; 95% confidence interval [CI], 53.6% - 62.1%) reported working at least once while sick in the previous year, and nearly one third (31.3%; 95% CI, 27.2% - 35.2%) reported working more than once while sick. More than half (52.9%; 95% CI, 48.5% - 57.1%) reported having insufficient time to visit a physician during the previous academic year.
Presenteeism was reported more often during PGY-2 (62.3%; 95% CI, 57.1% - 68.4%) than during PGY-1 (51.7%; 95% CI, 45.6% - 57.9%; P = .01). Sex, specialty, or medical school location did not affect reported rates of presenteeism or of having time to see a physician. Presenteeism rates did not vary significantly by hospital response rate or across hospitals, except for 1 outlier hospital in which 100% of residents reported working when sick.
"Despite major residency reforms over the last decade to ensure resident and patient health, rates of resident presenteeism were high and similar to rates observed in 1999," the study authors write. "The higher rate of reporting working when ill among PGY-2 vs. PGY-1 residents may reflect a greater responsibility toward patient care, consistent with higher presenteeism rates among workers who believe their duties are not easily substituted. The lack of factors associated with presenteeism suggests it may be pervasive."
Limitations of this study include reliance on self-report, lack of distinction between infectious and noninfectious illness, and potential bias associated with H1N1 influenza cases during survey development.
"Residents may work when sick for several reasons, including misplaced dedication, lack of an adequate coverage system, or fear of letting down teammates," the study authors conclude. "Regardless of reason, given the potential risks to patients related to illness and errors, resident presenteeism should be discouraged by program directors."
This study was funded by the Accreditation Council for Graduate Medical Education. Several of the study authors report various financial relationships with the Agency for Health Care Research and Quality, the National Institutes of Health, the Accreditation Council for Graduate Medical Education, the American Board of Internal Medicine Foundation, and/or the Institute of Medicine.
JAMA. 2010;304:1166-1168.
September 17, 2010
But the researchers emphasize they are not suggesting anyone get out of the pool. "We do not say stop swimming," says researcher Manolis Kogevinas, MD, PhD, professor of epidemiology at the Centre for Research in Environmental Epidemiology in Barcelona. "We should keep a clear message that swimmers should keep swimming."
The research findings, he tells WebMD, are a message to the industry that ''the positive effects of swimming could be increased by reducing the chemicals."
Industry experts and pool researchers agree. "It's good that research is being done in this area,'' says Thomas Lachocki, CEO of the National Swimming Pool Foundation, an educational nonprofit organization based in Colorado Springs, Colo. The research is published online in the journal Environmental Health Perspectives.
Swimming and Health Risks: A Closer Look
''We have been doing research on chemicals in water -- not swimming pools [specifically] -- for quite some time," Kogevinas says. More recently, he and his colleagues have focused more intently on indoor swimming pool water. "Chemicals are produced when you put chlorine in water," he says. Chlorine reacts, for instance, to urine, cosmetics, and other substances typically found in swimming pools.
The researchers wanted to characterize these disinfection byproducts, or DBPs, in an indoor pool environment. Other studies have linked DBP exposure in drinking water to a risk of bladder cancer and other problems.
In the first of three new studies published in the journal, the researchers evaluated 49 healthy adults after they swam for 40 minutes in an indoor chlorinated pool, looking for biomarkers linked to cancer.
"What we found is by analyzing blood samples and urine samples, we have an increase in risk markers related to cancer," Kogevinas tells WebMD.
Exposure to the pool water was associated with a five-fold increase in one of the markers, he says. But that does not mean swimmers are doomed to get cancer, he stresses.
"This doesn't mean at all that swimmers have a five times increased cancer risk," he says. "It simply means that after swimming for 40 minutes in a chlorinated pool, you get an increase in this marker in the blood that in other studies has been associated with future cancer risk."
Swimming and Respiratory Effects
In a second study, Kogevinas and his colleagues focused on respiratory effects of exposure to indoor pool water.
"We compared markers of lung injury before and after swimming," he says, evaluating 48 swimmers this time, from the same group as in the first study.
They found changes in just one blood marker, a slight increase in one known as CC16. The increase, the researchers say, is due to the exercise itself in addition to the DBP exposure.
''Some studies have suggested a link with swimming and asthma," Kogevinas says. "We found [only] one of many [respiratory] biomarkers [had] a small increase."
Swimming Pool Chemicals: What's in Pool Water?
In a third study, the researchers looked at water and air samples from two indoor pools. "We shipped them to the EPA [U.S. Environmental Protection Agency]," Kogevinas says. They found more than 100 DBPs in the pool water, some not identified before.
''Many are the same chemicals we find in tap water," he tells WebMD. "Some have been identified in experimental studies, animal studies, to be harmful."
The bottom line? "Pool water is not worse or better than tap water," he says, when it comes to byproducts. Only in the pool, he adds, "swimmers get a massive dose."
Swimming Pools and Health Risks: Second Views
Experts from the swimming pool industry say research is crucial. "It's important we find ways to reduce exposure to potentially hazardous chemicals in pools," Lachocki says.
Even so, he calls the three studies "limited" because of some shortcomings. He wanted more information on how the pools studied were managed and what standards were used to keep the pools maintained.
"The question is, were the pools studied on the end of the spectrum of fabulously well taken care of, or not so fabulously?" he says.
The conclusion of the research that the pool water is no more hazardous than drinking water doesn't tell people if that is representative of most pools or just the ones studied, Lachocki says.
Another limitation is the small number of swimmers studied, he says.
What's a Swimmer to Do?
Lachocki agrees that no one should give up swimming as a result of the research. "Swimming continues to be ideal for an aging population and for a sedentary population," he says.
People who swim in indoor pools can check out the pool first, he tells WebMD. Ask, for instance, if the pool has certified operators, which means they have had training in how best to disinfect a pool.
His foundation trains certified operators. "There should be a certificate on the wall, showing the people who operate the pool are certified."
Swimmers can buy test strips, widely available at pool supply stores, and test the water themselves, he says. Swimmers can also ask the pool operators to show them the maintenance records proving the pool is maintained properly, he says.
Kogevinas suggests that people who swim in indoor pools follow rules, such as not urinating in the pool and showering before swimming.
SOURCES:
Manolis Kogevinas, MD, PhD, professor of epidemiology, Centre for Research in Environmental Epidemiology, Barcelona, Spain.
Thomas Lachocki, PhD, CEO, National Swimming Pool Foundation, Colorado Springs, Colo.
Kogevinas, M. Environmental Health Perspectives, online Sept. 12, 2010.
Font-Ribera, L. Environmental Health Perspectives, online Sept. 12, 2010.
Richardson, S. Environmental Health Perspectives, online Sept. 12, 2010.
September 10, 2010
Presenting the study at last week's European Society of Cardiology (ESC) 2010 Congress, Dr Gunnar Gislason (Gentofte University Hospital, Hellerup, Denmark) said the results could have "massive public-health implications."
"First we found an increased risk of MI with NSAIDs. Now we are finding the same thing for stroke. This is very serious, as these drugs are very widely used, with many available over the counter," Gislason told heartwire . "We need to get the message out to healthcare authorities that these drugs need to be regulated more carefully."
Cochair of the session at which the study was presented, Dr Robert Califf (Duke Clinical Research Institute, Durham, NC), agreed that the results raised a major public-health issue, especially in the US, where many NSAIDs were available without a prescription.
For the current study, Gislason and colleagues examined the risk of stroke and NSAID use in healthy individuals living in Denmark. He explained to heartwire that information on each individual in the Danish population is kept in various national registries. His team started with the whole population of Denmark aged over 10 years. To select just the healthy individuals, they excluded anyone admitted to the hospital within the past five years or those prescribed chronic medications for more than two years. This left a population of around half a million, who were included in the study. By linking to prescribing registries, the researchers found that 45% of these healthy individuals had received at least one prescription for an NSAID between 1997 and 2005. They then used stroke data from further hospitalization and death registries and estimated the risk of fatal and nonfatal stroke associated with the use of NSAIDs by Cox proportional-hazard models and case-crossover analyses.
Results showed that NSAID use was associated with an increased risk of stroke. This increased risk ranged from about 30% with ibuprofen and naproxen to 86% with diclofenac.
Risk of Stroke With Various Nsaids
| NSAID | HR (95% CI) for risk of stroke |
| Ibuprofen | 1.28 (1.14–1.44) |
| Diclofenac | 1.86 (1.58–2.19) |
| Rofecoxib | 1.61 (1.14–2.29) |
| Celecoxib | 1.69 (1.11–2.26) |
| Naproxen | 1.35 (1.01–1.79) |
He conceded that his results could have some confounding but noted that the data were controlled for age, gender, and socioeconomic status and the patient population did not include those with chronic diseases. "We also have to think about the degree of confounding needed to nullify risk. It would have to increase risk four- to fivefold, which is very unlikely," he commented.
He said he did not find the results that surprising in view of the accumulating evidence of increased MI risk with these drugs, adding that the mechanism was probably the same. There have been several hypotheses about the mechanism linking NSAIDs with cardiovascular events, including increased thrombotic effect on platelets, the endothelium, and/or atherosclerotic plaques; increasing blood pressure; and effect on the kidneys and salt retention.
Gislason told heartwire that there is reluctance among the medical profession to limit the prescribing of these drugs. "The problem is that we don't have randomized trials, and it is very hard to change the habits of doctors. They have been using these drugs for decades without thinking about cardiovascular side effects."
He also stressed that the public needs to be protected by not allowing NSAIDs to be bought without a prescription. He has had some success in this regard in Denmark at least, where diclofenac became available over the counter recently, but after some of the MI data came out, Gislason's group campaigned the health authorities, and it has now become a prescription-only drug again. But he noted that many more NSAIDs are available over the counter in the US.
He believes the harmful effects of these agents are relevant to huge numbers of people. "If half the population takes these drugs, even on an occasional basis, then this could be responsible for a 50% to 100% increase in stroke risk. It is an enormous effect."
These results have been partly published in Circulation: Cardiovascular Quality and Outcomes earlier this year [1]. Gislason told heart wire that the novelty of the results presented at the ESC meeting was that "we had further analyzed our data regarding specific stroke and looked at the risk of ischemic stroke, and we confirmed that the risk of ischemic stroke was substantially elevated." He added: "We are in the process of analyzing these data related to time to risk and the effect of duration of treatment on stroke risk."
India embarks on one of the world's most ambitious vaccine rollouts after emergency use approval
(CNN)India is embarking on one of the world's most ambitious mass immunization programs ever undertaken after regulators approved the country's first two Covid-19 vaccines for restricted emergency use.

Mass vaccination drive

Lack of data

Vaccine rollouts in Asia
SARS-CoV-2 transmission role of mask in classroom setting
The University of Wisconsin-Madison has conducted a study showing that wearing facemasks in the classroom setting can be highly effective at reducing the aerosol transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).

However, the filtration efficiency of facemasks can below if they are not fitted properly, warns David Rothamer and colleagues.
The researchers also demonstrated that classroom ventilation alone did not sufficiently reduce the infection probability, whereas even the use of only moderately effective facemasks did reduce this probability sufficiently.
"The results reinforce the use of properly donned masks to achieve reduced aerosol transmission of SARS-CoV-2 and other infectious diseases transmitted via respiratory aerosol indoors," writes the team.
A pre-print version of the paper is available on the medRxiv* server while the article undergoes peer review.
Using the Wells-Riley equation to assess aerosol transmission
Since the first cases of SARS-CoV-2 were identified in Wuhan, China late last year (2020), researchers have increasingly recognized the long-range airborne route of viral transmission and the need for effective measures to block this transmission mode.
A common approach for assessing long-range airborne transmission (referred to hereafter as aerosol transmission), uses the Wells-Riley equation to relate aerosol concentrations to infection probability.
This approach has already been widely applied in studies of SARS-CoV-2, particularly in the context of super-spreader events.
The researchers say the application of the Wells-Riley equation is useful for risk assessment and the planning of interventions to reduce the risk of disease transmission.
"One of the aims of this paper is to provide recommendations that, when implemented, can decrease the likelihood of COVID-19 transmission in traditionally high occupancy spaces such as classrooms," they write.
What did the researchers do?
The team applied the Wells-Riley equation to evaluate the effect of ventilation, mask filtration, and a combination of the two on aerosol SARS-CoV-2 infection probability in the classroom setting.
Related Stories
A polydisperse neutralized salt (NaCl) aerosol that was generated in a size range consistent with SARS-CoV-2-containing bioaerosols was used as a safe surrogate for measurements.
The mask effective filtration efficiency was tested by seeding a classroom with the NaCl aerosol and sampling concentrations of the aerosol through four different mask types that had been fitted to manikins with and without using mask fitters.
Two of the masks were washable reusable masks. One was made of 4-layers of knit cotton, and the other was made of 3-layers of non-woven spun-bond polypropylene.
The other two masks were disposable. One was a common single-use disposable mask (referred to hereafter as procedure mask), and the other was an ASTM F2100 level-2 surgical mask.
The importance of masks fitting properly
Measurements of the mask's effective filtration efficiency demonstrated the importance of masks being fitted properly. Poorly fitting masks exhibited filtration efficiencies that decreased by as much as a factor of six. The estimated leakage rate for most of the poorly fitted masks was typically more than 50%.
The analysis also found that the knit-cotton mask was only able to achieve an effective filtration efficiency of 26%, even when a mask fitter was used.
In all other cases, the use of a mask fitter significantly improved the effective filtration efficiency, with the exception of the polypropylene mask, which achieved a good fit without a mask fitter. In the case of the procedure mask, the use of a mask fitter achieved effective filtration efficiencies of almost 95%.
Classroom ventilation alone was insufficient
The study also suggested that classroom ventilation alone was not sufficient to achieve infection probabilities of less than 1%.
On the other hand, the use of moderate-to-high effective filtration efficiency masks by all individuals (manikins) present significantly reduced the infection probability.
Depending on the type of mask and whether a mask fitter was used, infection probability was reduced by 5-, 10- or even more than 100-fold.
The team says infection probabilities of less than 0.1% and even lower than 0.0001% could be reached with the use of masks and mask fitters alone.
What does the team advise?
Rothamer and colleagues say the results reinforce the use of properly donned masks to achieve reduced aerosol transmission of SARS-CoV-2.
"The results specifically emphasize the large potential for effective mask-wearing and improved masks, or use of mask fitters, to greatly reduce infection probabilities," concludes the team.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Rothamer D, et al. Strategies to minimize SARS-CoV-2 transmission in classroom settings: Combined impacts of ventilation and mask effective filtration efficiency. medRxiv, 2020. https://www.medrxiv.org/content/10.1101/2020.12.31.20249101v1
OBESITY
What Causes Obesity?
"What causes a person to become obese?"
Obesity occurs when, over a long period of time, the amount of food we put into our bodies each day is not used. In essence, this means that there consistently is more energy going in, than out. That energy has to go somewhere, so our bodies store it as fat.
Energy In vs Energy Out Equation
ENERGY "IN" MORE THAN ENERGY "OUT" = WEIGHT GAIN.
ENERGY "IN" LESS THAN ENERGY "OUT" =WEIGHT LOSS.
We all overindulge every now and then, and it isn’t this occasional overeating that causes obesity; obesity is caused when we overdo it most days, for a sustained period of time.
Unfortunately, we live in an environment that encourages us to eat and discourages us to be active, making it very easy to gain weight.
Have a think about it…
Food is readily available, 24 hours a day, 7 days a week Portion sizes and plates are much bigger than they have been before we can get almost anywhere without having to walk or use a bikeTVs, computers and mobile phones encourage a more sedentary lifestyle.
Smoking Ban Reduces Childhood Asthma Hospital Admissions
Daniel Mackay, PhD, from the University of Glasgow, in Scotland, and colleagues reported the findings in the September 16 issue of the New England Journal of Medicine.
According to the researchers, the Smoking, Health and Social Care (Scotland) Act banned smoking in all enclosed public places and workplaces in Scotland as of March 26, 2006.
"The legislation has been extremely successful in its primary aim of reducing exposure to environmental tobacco smoke in public places, such as bars," the authors note. In addition, the legislation has reduced exposure of children to environmental tobacco smoke, despite concerns of smoking being displaced to the home, but it is unclear whether the risk for childhood asthma has also decreased.
The researchers collected routine hospital administrative data and ascertained all hospital admissions for asthma in Scotland from January 2000 through October 2009 among children younger than 15 years.
Before the smoking ban, asthma admissions were increasing by an average of 5.2% per year (95% confidence interval [CI], 3.9% - 6.6%). After the ban, the rate of admissions decreased by 18.2% per year relative to the rate on March 26, 2006 (95% CI, 14.7% to 21.8%; P < .001). Rates were reduced both in preschool and school-age children.
Various factors including age group, sex, urban or rural residence, region, or quintile of socioeconomic status had no effect on the outcome.
Limitations of the study include that only exacerbations severe enough to warrant hospitalization were included. In addition, information regarding individual smoking status was not available; therefore, whether the observed reduction in asthma was a result of reduced exposure to environmental tobacco smoke in the home, reduced exposure to environmental tobacco smoke in public places, a reduction in active smoking among school-age children, or an unrelated cause cannot be determined.
"After the introduction of comprehensive smoke-free legislation, there was a reduction in the incidence of asthma among people who did not have occupational exposure to environmental tobacco smoke," the authors conclude.
They add that the "overall exposure of children to environmental tobacco smoke, measured objectively with the use of salivary cotinine concentrations, has fallen since the implementation of the Scottish legislation."
The study was supported by a project grant from National Health Services Health Scotland. One author reports individual employment by National Health Services Scotland; another chairs the Committee on Medical Effects of Air Pollution for the UK Department of Health. The other authors have disclosed no relevant financial relationships.
N Engl J Med. 2010;363:1139-1145.
Nearly Half of Infected US Gay and Bisexual Men Unaware They Have HIV
"[MSM] are at increased risk for infection with [HIV]," write A. Smith, MPH, and colleagues from the Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, US Centers for Disease Control and Prevention (CDC). "In 2006, 57% of new HIV infections in the United States occurred among MSM."
The CDC uses the National HIV Surveillance system (NHBS) to monitor prevalence and trends in HIV-related risk behaviors, HIV testing, and use of HIV prevention services among high-risk populations. In the current report, the authors summarize NHBS data from 2008.
From January to December 2008, 8153 MSM from 21 cities were interviewed and tested for HIV. The study found that the overall prevalence of HIV was 19%.
Non-Hispanic blacks had the highest prevalence (28%), followed by Hispanics (18%), non-Hispanic whites (16%), and persons who were multiracial or of other race (17%).
Forty-four percent of those infected with HIV were unaware of their status. Black MSM with HIV were least likely to be aware of their infection (59%), followed by Hispanic MSM (46%) and white MSM (26%).
The study also found that although young men, aged 30 years or younger, had a lower HIV prevalence than older men, they were much more likely to be unaware of their HIV infection. Among men aged 18 to 29 years who had HIV, 63% were unaware vs 37% of men aged 30 years and older.
Also among young men, MSM of color were less likely than their white counterparts to know they were infected with HIV. Among blacks aged 30 years or younger, 71% were unaware of their status compared with 63% of young Hispanic MSM and 40% of young white MSM.
The study also found a strong link between socioeconomic status and HIV infection in MSM. The prevalence of HIV infection increased as education and income decreased, as did awareness. These findings are similar to those found in recent NHBS research among homosexuals, the authors report.
Men who know their current HIV infection status can be referred to appropriate medical care and prevention services. Once they are linked to prevention services, they can learn ways to avoid transmitting HIV to others, the authors note, adding that efforts to reach out to young and minority MSM should be increased to promote testing for HIV.
The authors also note limitations of their report. Because interviewers conducted the surveys, positive HIV status might have been underreported. Also, because the findings are limited to men who frequented bars, dance clubs, and other MSM venues, they may not be representative of results for all MSM.
"The high proportion of MSM unaware of their HIV infection continues to be a serious public health concern, because these MSM account for the majority of estimated new HIV transmissions in the United States," the author write in their concluding remarks. "The 2008 NHBS data show that MSM remain a key target of strategies to reduce HIV incidence and decrease racial and socioeconomic disparities in the United States."
"This study's message is clear: HIV exacts a devastating toll on [MSM] in America's major cities, and yet far too many of those who are infected don't know it," Kevin Fenton, MD, director of the CDC's National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said in a statement. "We need to increase access to HIV testing so that more MSM know their status, and we all must bring new energy, new approaches, and new champions to the fight against HIV among [MSM]."
The authors have disclosed no relevant financial relationships.
Morb Mortal Wkly Rep. 2010;59:1201-1207
Depression Plus Heart Disease a Particularly Lethal Combination
Compared with patients without depression and CHD, the risk for all-cause mortality was 3 times higher, and the risk for cardiovascular disease mortality 4 times higher, in patients who had both, after adjusting for age and sex, report Hermann Nabi, MD, from Hôpital Paul-Brousse, Villejuif, Paris, France, and colleagues.
"This study provides further evidence that the relationship between depression and morbidity–mortality is real," Dr. Nabi told Medscape Medical News.
Depression and mortality have been studied separately in patients with CHD and in healthy patients, but this does not allow comparisons across risk-factor groups according to depression and CHD status.
In the study, Dr. Nabi and his team examined the effects of both on mortality in 5936 middle-aged men and women whose mental and physical health were followed-up for a mean of 5.6 years.
The study population was part of the Whitehall II cohort study, a longitudinal study established in 1985 to examine the effect of social and economic factors on the long-term health of 10,308 civil servants who were aged between 35 and 55 years at the start of the study.
Of the 5936 individuals, 170 died during follow-up; 47 of those deaths were from cardiovascular disease.
The analysis showed that the prevalence of depression was 14.9%, and participants with a history of CHD were more likely to have depressive symptoms (20% vs 14%; P = .001) than those without CHD.
The age- and sex-adjusted hazard ratios for all-cause mortality were 1.67 (P < .05) for participants with CHD only, 2.10 (P < .001) for those with depressive symptoms only, and 4.99 (P < .001) for those with both CHD and depressive symptoms compared with participants who were free of both conditions.
Need for a More Integrated Approach
The study findings have implications for research and clinical practice, Dr. Nabi said.
"For research, this study shows that the mechanisms underlying the association between depression and adverse health outcomes such as mortality are still in need of comprehensive studies."
For clinical practice, it implies the need for a more integrated approach in the healthcare system and a shift toward a more "mind–body medicine' approach.
An important step would be to identify cardiac patients who also have depression, he said.
"In this study, the depression worsened heart disease, because we observed that participants with both depression and heart disease were at increased risk for death when compared with those with heart disease only. So we should identify those cardiac patients who have clinically significant depressive symptoms."
Dr. Nabi expressed the wish that his study findings will prompt clinicians to be aware of and look for depression in their patients with heart disease.
"Even though there is no consensus at the moment, healthcare professionals should screen and treat, or refer to treatment. Simple screening tools exist, and [clinicians] should refer their depressed patients, particularly if an adequate referral for systematic depression assessment and treatment is readily available."
He also discussed some limitations of the study.
"This study is based on a cohort of civil servants and did not include blue-collar workers, unemployed, or individuals with precarious jobs. This may have underestimated the magnitude of associations observed in our study because of the prevalence of depression and the mortality rate is higher in these latter individuals. Thus, it is reasonable to assume that the effect of depression would be greater in studies including various populations."
Randomized Trial Required
"This paper is adding to a literature that is imperfect. It makes you feel more confident about the literature," Alexander H. Glassman, MD, chief of clinical psychopharmacology at New York State Psychiatric Institute and professor of psychiatry at Columbia University, New York City, commented to Medscape Medical News.
"There are literally a hundred, maybe more, studies indicating that depression and heart disease are related," Dr. Glassman, who was not part of the current study, noted. "There are a handful of studies that do not find a relationship, but they are vastly outnumbered by the ones that have found a relationship."
However, he pointed out, just because there is an association that does not mean one condition causes the other. The way to prove cause would be with a randomized controlled trial.
"It's very easy to think depression is increasing the risk or is a cause of subsequent heart disease. And let me say, I think it is," said Dr. Glassman, who led the placebo-controlled Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), as reported by Medscape Medical News.
SADHART found that patients hospitalized for acute coronary syndrome who also have major depression are twice as likely to die within 7 years if their depression did not significantly improve.
"The best way to know for sure would be to do a randomized trial on the treatment for depression with a placebo control. If you reduced the depression and those people with an antidepressant effect had a lower mortality, then you would have unequivocal evidence that depression is causing death, because by getting rid of it, you reduce the chance of dying."
The study was funded by the Medical Research Council, British Heart Foundation, Health and Safety Executive, Department of Health, National Heart Lung and Blood Institute, National Institute on Aging, Agency for Health Care Policy Research, and John D. and Catherine T. MacArthur Foundation Research Networks on Successful Midlife Development and Socio-economic Status and Health. Dr. Nabi has disclosed no relevant financial relationships. Dr. Glassman reports financial relationships with Pfizer Inc.
Heart. Published online September 16, 2010.
Women With Low Sexual Arousal May Have Symptom Changes With Placebo Treatment
"In clinical trials of drug treatments for women's sexual dysfunction, placebo responses have often been substantial," write Andrea Bradford, PhD, from Baylor College of Medicine in Houston, Texas, and Cindy M. Meston, PhD, from the University of Texas at Austin. "However, little is known about the clinical significance, specificity, predictors, and potential mechanisms of placebo response in sexual dysfunction."
The goal of the study was to evaluate the characteristics and predictors of sexual function outcomes in 50 women with FSAD who were randomly assigned to the placebo group of a 12-week, multisite, controlled pharmaceutical trial. Magnitude, domain specificity, and clinical significance of sexual function scores were evaluated at baseline and at 4, 8, and 12 weeks (after study completion).
Change with time in sexual function outcomes was assessed in relationship to several variables, including age and symptom-related distress at baseline, as well as changes in frequency of sexual behavior during the trial. The primary study endpoint was the total score on the Female Sexual Function Index.
"It's important to note that, even though these women received placebo, they all had an opportunity to talk to a health provider about their difficulties and were asked to closely monitor their sexual behavior and feelings over a 12-week period," Dr. Bradford said in a news release. "Just taking part in this study probably started some meaningful conversations."
Approximately one third of women receiving placebo had a clinically significant magnitude of change after study completion, with similar effect sizes across multiple aspects of sexual function. Although symptom improvement was strongly associated with the frequency of satisfying sexual encounters (SSEs) during treatment, there was significant variation between participants in the association between frequency of sexual encounters and outcome.
"Our study shows that even a limited intervention can have a positive effect in many women with sexual dysfunction," Dr. Bradford said. "This comes as no surprise to sex therapists, but it does suggest a need to investigate behavioral factors more closely in clinical trials."
Limitations of this study include observational design, precluding determination of causality; and the possibility that SSE frequency was just a proxy for another variable, such as changes in general relationship functioning. In addition, the retrospective analysis prevented direct manipulation of variables of interest, and it is not known whether trial participants who received no treatment would have reported the same effects as participants who received placebo.
"A substantial number of women experienced clinically significant improvement in sexual function during treatment with placebo," the study authors write. "Changes in sexual behavior during the trial, more so than participant age or symptom severity at baseline, appeared to be an important determinant of outcome. Contextual and procedural aspects of the clinical trial may have influenced outcomes in the absence of an active drug treatment."
Eli Lilly/ICOS shared the data set used in this study. This study was supported in part by the Houston VA HSR&D Center of Excellence. The views expressed in the journal article are those of the study authors and do not necessarily represent the views of the Department of Veterans Affairs. Drs. Bradford and Meston have disclosed no relevant financial relationships.
J Sex Med. Published online September 16, 2010.
Weight Control and Exercise Could Prevent 20% of Colon Cancer
The data are reported in the September issue of the European Journal of Cancer, which is dedicated to cancer prevention.
An increasing proportion of the European population now has a body mass index (BMI) higher than 25 kg/m2, and few Europeans are engaging in the amounts of physical activity recommended by current guidelines (at least 30 minutes of moderate-intensity activity 5 or more days a week), the researcher note.
The researchers set out to predict what would happen if the European population managed to maintain a mean BMI of 21 kg/m2 and if all countries had a level of physical activity similar to that seen in the Netherlands, where both cycling and walking are popular.
They used the PREVENT statistical modeling method, which was developed at Erasmus University in the Netherlands and is frequently used in the European Union's EUROCADET project.
"We know that large numbers of colon cancer cases could be avoided by reducing exposure to risk factors," said senior author Andrew Renehan, PhD, FRCS, FDS, from the School of Medicine, University of Manchester, United Kingdom. And 2 of the most easily controllable risk factors are physical inactivity and excess weight, he added.
"The predictive modeling is beginning to tease out the independent relevance of each of these factors in the prevention of colon cancer," he said in a statement.
"Preventing weight gain and encouraging weight reduction seem to be most beneficial in men, but for women a strategy with a greater emphasis on increasing physical activity would be more effective," he explained.
Colon Cancer Increasing
Colon cancer rates are increasing in Europe; they have been on the rise since 1975. It is the second most common cancer in Europe and the second most common cause of cancer death, the researchers note.
In a previous study, Dr. Renehan and colleagues attributed the increasing rates of all cancers to increasing obesity in European countries. They estimated that in 2008, new cancers attributed to excess body weight affected 3.2% of women and 8.6% of men; this was an increase from the estimates for 2002, which projected that excess weight was related to new cancers in 2.5% of men and 4.1% of women.
Those data were presented at the 2009 meeting of the European Cancer Organization, and reported by Medscape Medical News at the time.
"People in Europe are gaining weight," Dr. Renehan said at the time, "and it is projected to keep rising."
In the new study, the researchers used the computer model to look at what would happen if Europeans continued to grow fatter, using a hypothetical scenario in which obesity levels increased at the same rate as they have in the United States. They predicted that this would lead to an increase in the number of new colon cancer cases of between 0.7% and 3.8%, depending on the European country.
Then they hypothesized a scenario in which Europeans managed to control their weight and managed to achieve an optimum BMI of 21 kg/m2. They calculated that by the year 2040, this weight-control strategy would prevent between 2% and 18% of colon cancer cases across the countries they studied. The benefits were much higher for males (13.5% to 18%) than for females (2.3% to 4.6%), and most benefit would be seen in British males (in whom 18% of new colon cancer cases could be prevented).
This "underlines the importance of stopping and reversing the ongoing increase in overweight and obesity prevalence," the authors note.
When the team considered physical activity, they found that the Netherlands had the highest rates, which they attributed to a high frequency of bike use, often as a means of transportation. They also found high levels of walking.
Using the Netherlands as the ideal, the researchers predicted what would happen if other countries adopted the same amount of physical activity. They found that overall, 17.5% of new colon cancer cases could be prevented by 2040, with the most benefit in Spanish females (in whom 21% of new colon cancer cases could be prevented).
"We can safely say that increasing physical activity across Europe to the level already achieved in the Netherlands, where everyone cycles, would be of substantial benefit," said coauthor Jan-Willem Coebergh, MD, PhD, from Erasmus University.
"In summary, the changes in physical activity and/or mean levels of overweight in the selected European populations would result in quite substantial effects on future colon cancer rates," the authors conclude.
The researchers have disclosed no relevant financial relationships.
Eur J Cancer. 2010;46:2605-2616.
Resident Physicians Have High Rates of Presenteeism (Working While Sick)
"Despite recent Centers for Disease Control and Prevention guidelines urging health care personnel with flu-like illness to avoid working, presenteeism (working while sick) is prevalent among health care workers," write Anupam B. Jena, MD, PhD, from Massachusetts General Hospital in Boston, and colleagues. "Ill health care workers can endanger patients and colleagues due to decline in performance or spread of disease. Resident physicians may face unique pressures to work when sick and lack time to seek health care."
The study goal was to evaluate self-reported presenteeism rates and associated factors among residents in a sample of programs selected for varied geographic, size, and governance characteristics. A 50-item survey was administered anonymously in August 2009 to 744 residents in postgraduate year (PGY) 2 and 3 in general surgery, obstetrics/gynecology, internal medicine, and pediatrics at 35 programs in 12 hospitals regarding presenteeism during the prior year. Overall response rate was 72.2% (range among hospitals, 48% - 100%).
More than half of responders (57.9%; 95% confidence interval [CI], 53.6% - 62.1%) reported working at least once while sick in the previous year, and nearly one third (31.3%; 95% CI, 27.2% - 35.2%) reported working more than once while sick. More than half (52.9%; 95% CI, 48.5% - 57.1%) reported having insufficient time to visit a physician during the previous academic year.
Presenteeism was reported more often during PGY-2 (62.3%; 95% CI, 57.1% - 68.4%) than during PGY-1 (51.7%; 95% CI, 45.6% - 57.9%; P = .01). Sex, specialty, or medical school location did not affect reported rates of presenteeism or of having time to see a physician. Presenteeism rates did not vary significantly by hospital response rate or across hospitals, except for 1 outlier hospital in which 100% of residents reported working when sick.
"Despite major residency reforms over the last decade to ensure resident and patient health, rates of resident presenteeism were high and similar to rates observed in 1999," the study authors write. "The higher rate of reporting working when ill among PGY-2 vs. PGY-1 residents may reflect a greater responsibility toward patient care, consistent with higher presenteeism rates among workers who believe their duties are not easily substituted. The lack of factors associated with presenteeism suggests it may be pervasive."
Limitations of this study include reliance on self-report, lack of distinction between infectious and noninfectious illness, and potential bias associated with H1N1 influenza cases during survey development.
"Residents may work when sick for several reasons, including misplaced dedication, lack of an adequate coverage system, or fear of letting down teammates," the study authors conclude. "Regardless of reason, given the potential risks to patients related to illness and errors, resident presenteeism should be discouraged by program directors."
This study was funded by the Accreditation Council for Graduate Medical Education. Several of the study authors report various financial relationships with the Agency for Health Care Research and Quality, the National Institutes of Health, the Accreditation Council for Graduate Medical Education, the American Board of Internal Medicine Foundation, and/or the Institute of Medicine.
JAMA. 2010;304:1166-1168.
Swimming Pool Chemicals May Carry Cancer Risk
But the researchers emphasize they are not suggesting anyone get out of the pool. "We do not say stop swimming," says researcher Manolis Kogevinas, MD, PhD, professor of epidemiology at the Centre for Research in Environmental Epidemiology in Barcelona. "We should keep a clear message that swimmers should keep swimming."
The research findings, he tells WebMD, are a message to the industry that ''the positive effects of swimming could be increased by reducing the chemicals."
Industry experts and pool researchers agree. "It's good that research is being done in this area,'' says Thomas Lachocki, CEO of the National Swimming Pool Foundation, an educational nonprofit organization based in Colorado Springs, Colo. The research is published online in the journal Environmental Health Perspectives.
Swimming and Health Risks: A Closer Look
''We have been doing research on chemicals in water -- not swimming pools [specifically] -- for quite some time," Kogevinas says. More recently, he and his colleagues have focused more intently on indoor swimming pool water. "Chemicals are produced when you put chlorine in water," he says. Chlorine reacts, for instance, to urine, cosmetics, and other substances typically found in swimming pools.
The researchers wanted to characterize these disinfection byproducts, or DBPs, in an indoor pool environment. Other studies have linked DBP exposure in drinking water to a risk of bladder cancer and other problems.
In the first of three new studies published in the journal, the researchers evaluated 49 healthy adults after they swam for 40 minutes in an indoor chlorinated pool, looking for biomarkers linked to cancer.
"What we found is by analyzing blood samples and urine samples, we have an increase in risk markers related to cancer," Kogevinas tells WebMD.
Exposure to the pool water was associated with a five-fold increase in one of the markers, he says. But that does not mean swimmers are doomed to get cancer, he stresses.
"This doesn't mean at all that swimmers have a five times increased cancer risk," he says. "It simply means that after swimming for 40 minutes in a chlorinated pool, you get an increase in this marker in the blood that in other studies has been associated with future cancer risk."
Swimming and Respiratory Effects
In a second study, Kogevinas and his colleagues focused on respiratory effects of exposure to indoor pool water.
"We compared markers of lung injury before and after swimming," he says, evaluating 48 swimmers this time, from the same group as in the first study.
They found changes in just one blood marker, a slight increase in one known as CC16. The increase, the researchers say, is due to the exercise itself in addition to the DBP exposure.
''Some studies have suggested a link with swimming and asthma," Kogevinas says. "We found [only] one of many [respiratory] biomarkers [had] a small increase."
Swimming Pool Chemicals: What's in Pool Water?
In a third study, the researchers looked at water and air samples from two indoor pools. "We shipped them to the EPA [U.S. Environmental Protection Agency]," Kogevinas says. They found more than 100 DBPs in the pool water, some not identified before.
''Many are the same chemicals we find in tap water," he tells WebMD. "Some have been identified in experimental studies, animal studies, to be harmful."
The bottom line? "Pool water is not worse or better than tap water," he says, when it comes to byproducts. Only in the pool, he adds, "swimmers get a massive dose."
Swimming Pools and Health Risks: Second Views
Experts from the swimming pool industry say research is crucial. "It's important we find ways to reduce exposure to potentially hazardous chemicals in pools," Lachocki says.
Even so, he calls the three studies "limited" because of some shortcomings. He wanted more information on how the pools studied were managed and what standards were used to keep the pools maintained.
"The question is, were the pools studied on the end of the spectrum of fabulously well taken care of, or not so fabulously?" he says.
The conclusion of the research that the pool water is no more hazardous than drinking water doesn't tell people if that is representative of most pools or just the ones studied, Lachocki says.
Another limitation is the small number of swimmers studied, he says.
What's a Swimmer to Do?
Lachocki agrees that no one should give up swimming as a result of the research. "Swimming continues to be ideal for an aging population and for a sedentary population," he says.
People who swim in indoor pools can check out the pool first, he tells WebMD. Ask, for instance, if the pool has certified operators, which means they have had training in how best to disinfect a pool.
His foundation trains certified operators. "There should be a certificate on the wall, showing the people who operate the pool are certified."
Swimmers can buy test strips, widely available at pool supply stores, and test the water themselves, he says. Swimmers can also ask the pool operators to show them the maintenance records proving the pool is maintained properly, he says.
Kogevinas suggests that people who swim in indoor pools follow rules, such as not urinating in the pool and showering before swimming.
SOURCES:
Manolis Kogevinas, MD, PhD, professor of epidemiology, Centre for Research in Environmental Epidemiology, Barcelona, Spain.
Thomas Lachocki, PhD, CEO, National Swimming Pool Foundation, Colorado Springs, Colo.
Kogevinas, M. Environmental Health Perspectives, online Sept. 12, 2010.
Font-Ribera, L. Environmental Health Perspectives, online Sept. 12, 2010.
Richardson, S. Environmental Health Perspectives, online Sept. 12, 2010.
NSAID Use Associated With Future Stroke in Healthy Population
Presenting the study at last week's European Society of Cardiology (ESC) 2010 Congress, Dr Gunnar Gislason (Gentofte University Hospital, Hellerup, Denmark) said the results could have "massive public-health implications."
"First we found an increased risk of MI with NSAIDs. Now we are finding the same thing for stroke. This is very serious, as these drugs are very widely used, with many available over the counter," Gislason told heartwire . "We need to get the message out to healthcare authorities that these drugs need to be regulated more carefully."
Cochair of the session at which the study was presented, Dr Robert Califf (Duke Clinical Research Institute, Durham, NC), agreed that the results raised a major public-health issue, especially in the US, where many NSAIDs were available without a prescription.
For the current study, Gislason and colleagues examined the risk of stroke and NSAID use in healthy individuals living in Denmark. He explained to heartwire that information on each individual in the Danish population is kept in various national registries. His team started with the whole population of Denmark aged over 10 years. To select just the healthy individuals, they excluded anyone admitted to the hospital within the past five years or those prescribed chronic medications for more than two years. This left a population of around half a million, who were included in the study. By linking to prescribing registries, the researchers found that 45% of these healthy individuals had received at least one prescription for an NSAID between 1997 and 2005. They then used stroke data from further hospitalization and death registries and estimated the risk of fatal and nonfatal stroke associated with the use of NSAIDs by Cox proportional-hazard models and case-crossover analyses.
Results showed that NSAID use was associated with an increased risk of stroke. This increased risk ranged from about 30% with ibuprofen and naproxen to 86% with diclofenac.
Risk of Stroke With Various Nsaids
| NSAID | HR (95% CI) for risk of stroke |
| Ibuprofen | 1.28 (1.14–1.44) |
| Diclofenac | 1.86 (1.58–2.19) |
| Rofecoxib | 1.61 (1.14–2.29) |
| Celecoxib | 1.69 (1.11–2.26) |
| Naproxen | 1.35 (1.01–1.79) |
He conceded that his results could have some confounding but noted that the data were controlled for age, gender, and socioeconomic status and the patient population did not include those with chronic diseases. "We also have to think about the degree of confounding needed to nullify risk. It would have to increase risk four- to fivefold, which is very unlikely," he commented.
He said he did not find the results that surprising in view of the accumulating evidence of increased MI risk with these drugs, adding that the mechanism was probably the same. There have been several hypotheses about the mechanism linking NSAIDs with cardiovascular events, including increased thrombotic effect on platelets, the endothelium, and/or atherosclerotic plaques; increasing blood pressure; and effect on the kidneys and salt retention.
Gislason told heartwire that there is reluctance among the medical profession to limit the prescribing of these drugs. "The problem is that we don't have randomized trials, and it is very hard to change the habits of doctors. They have been using these drugs for decades without thinking about cardiovascular side effects."
He also stressed that the public needs to be protected by not allowing NSAIDs to be bought without a prescription. He has had some success in this regard in Denmark at least, where diclofenac became available over the counter recently, but after some of the MI data came out, Gislason's group campaigned the health authorities, and it has now become a prescription-only drug again. But he noted that many more NSAIDs are available over the counter in the US.
He believes the harmful effects of these agents are relevant to huge numbers of people. "If half the population takes these drugs, even on an occasional basis, then this could be responsible for a 50% to 100% increase in stroke risk. It is an enormous effect."
These results have been partly published in Circulation: Cardiovascular Quality and Outcomes earlier this year [1]. Gislason told heart wire that the novelty of the results presented at the ESC meeting was that "we had further analyzed our data regarding specific stroke and looked at the risk of ischemic stroke, and we confirmed that the risk of ischemic stroke was substantially elevated." He added: "We are in the process of analyzing these data related to time to risk and the effect of duration of treatment on stroke risk."